Change is inevitable, misery is optional
Read MoreReflections on GP training by Dr Batool Albatat
GPT1/GPT2 (General practice term 1/General practice term 2)
It's been a year since I started my journey as a general practitioner, and it's been an incredible experience. Initially, when I finished medical school, I wasn't sure which medical pathway to choose. I worked for a few years at the hospital as a medical officer, doing surgical, obstetrics & gynaecology, paediatrics and general medicine, enjoying every aspect of medicine, but not knowing which medical pathway to choose. General practice never seemed like an attractive option for me. I had all the worries and fears that I might not enjoy it and that I would just be sitting at my desk signing medical certificates and renewing prescriptions. But as soon as I dove into my work, I quickly realized it was the perfect fit for me.
Starting off was scary and very overwhelming. After orientation, I found myself alone with patients coming to see me. The responsibility and pressure of being the primary doctor was overwhelming. I was no longer a medical student, intern, or the hospital medical officer who was given instructions on how to manage patients. I was now the doctor, and the weight of that role was heavy. The imposter syndrome kicked in, and I felt like I didn't know what I was doing. I found myself constantly looking up guidelines and searching for information. But as time went on, I began to find my footing. The learning curve was steep, but also expansive. I discovered new things about medicine and about myself as a doctor. And as I continue on this amazing journey, I know that I will always be learning and growing.
The year was filled with a variety of patients and experiences. I've had the privilege of seeing women's health, performing simple procedures, treating paediatric and geriatric patients. GP may not be as "sexy" as other medical professions, and we are not often depicted in movies like "Scrubs" or "The Good Doctor," but we are the backbone of all medicine, and I am glad to be a part of this community of amazing colleagues.
Throughout my year as a GP, I've had the opportunity to share so many unique stories and provide as much care as possible to all different people from all walks of life. I've seen patients with alcohol addiction and walked alongside them on their withdrawal journey. I've reassured mothers and given them a listening ear. I've seen older patients and given them my time, my attention, and my care. I've seen patients in their most vulnerable states, opening up to me about their mental health, and placing their trust in me to guide them towards hope and healing. I've given immunizations to people of all ages, knowing that I am preventing them from getting ill in the future.
I've sent patients to the hospital for surgery and helped guide them through their recovery process post-surgery. I've done simple things like ear syringing, but with a big impact on my patients' hearing. I've done iron infusions and seen patients come back saying they feel amazing. I've seen so many undifferentiated diagnoses and followed up with patients throughout their journey with their symptoms. I've seen patients being diagnosed with cancer and have helped them and their families find the right medical pathway and treatment.
Through all of this, I've made strong connections with my patients and their families. Being chosen as their doctor is truly a privilege. It's been amazing how much I could help patients not just to survive, but to thrive. I was able to make a real difference in people's lives, and that was incredibly fulfilling. It's very rewarding for me to see my patients progress and to know that I played a small role in their journey towards recovery and well-being. I am thankful to the Lord for giving me this privilege to be a carer, provider, friend, and companion to so many people that I encounter daily in my life.
Being a GP is challenging at times, but it's fulfilling, heart-warming, and rewarding in many ways that I never imagined. Caring for my patients with empathy and fairness is a constant endeavor that has certainly been a big leap for me. But I feel proud to be part of the GP community and have joined an amazing group of colleagues who have the same dedication and passion for providing care to patients. I am grateful for this experience and look forward to many more years of providing care with passion.
Words by Dr Batool Albatat, images by Dr Wendy Burton
Dear dad in the park, this is why I’m not ‘just a GP’
It was nice to see you. A familiar face from the school playground, someone I’d not seen for three months during Melbourne’s lockdown.
We exchanged our socially distanced niceties while our children played.
‘So, how’s your work been?’ you asked, before adding, ‘Aren’t you a doctor?’
I nodded and started with my standard response, mentioning ‘very challenging times’ before moving to ‘we are in a much better position than so many other countries’.
But I didn’t get to finish before you interrupted me.
‘You’re just a GP, though, aren’t you?’
I froze.
Had you really said that? Would you have said the same to someone male? To someone older than me? To someone who hadn’t trained overseas?
Yes, I decided, you probably would.
As I began to challenge what you’d said, you interrupted me again to dig the hole deeper.
‘Well, you’re not a brain surgeon, are you?’
The smiles behind our masks faded. I let silence make my point. You were grateful for the intervention of your son who needed help on the swing. Later, you slunk from the park without a word, your children shouting objections behind you.
So, dad in the park, here’s what I really wanted to say. Here’s why we’re not ‘just’ GPs.
It starts well before university
We work hard, and not just at science and maths. We need to be good at other things to stand out from the thousands of other hopefuls. Sports, voluntary work, expeditions, work experience.
We juggle teenage hormones, first relationships and friendships with cramming for exams and interviews. If we get to university, we’re suddenly surrounded by hundreds of other competitive straight-A students just like us.
We see life – the raw, unedited version. Its gory beginnings, its undignified ends. The loops of pain, fear, grief, and joy that punctuate it along the way.
For some of us, that’s too much and other careers call. For those who finish the long years of medical school, there’s at least another four or five years of hospital shifts. For this, we’ll sacrifice holidays, family dinners, weddings, Christmases, Hanukkahs, Eids, Diwalis.
We’ll sacrifice relationships. We’ll fall asleep in cinemas, during dates, at roadsides driving home from a week of nightshifts. We’ll be haunted by our memories and experiences and wonder ‘what if’ and think ‘by the grace of God...’.
There’ll be songs we can’t listen to without crying. Mine is Wires by Athlete: it played on the radio as I drove home from my first – and unsuccessful – paediatric resuscitation. There’ll be faces and names and places and smells that haunt us.
Mine is the accidental double dosing of lithium, prescribed at 3.00 am after seven sleep-deprived night shifts. The patient survived, but the mistake still frequents my dreams.
And then, we’ll be GPs
Not ‘just’ GPs. Not ‘non-specialists.’ Specialists in primary care.
We’ve chosen to be one of the few remaining generalists. Not because we couldn’t be brain surgeons, or gastroenterologists or cardiologists, but because we chose not to be. Because we wanted patients who were awake and could talk to us, because we know that consultation skills are the heart of medicine. Because we want to treat bowel problems and neurological problems and heart problems, and everything else besides.
So, dad in the park, we’ll care for you and your family at every stage of life. We’ll provide contraceptive care. Not just ‘the pill’ – we can insert contraceptive implants and IUDs, too (some of us even do vasectomies).
If the time’s right, we’ll provide you and your partner with advice before conception, as well as first-trimester screening and antenatal care. We’ll carefully check your brand-new babies head to toe. We’ll vaccinate them against meningitis, measles, whooping cough, and more. We’ll treat their nappy rash, eczema, constipation, and ear infections.
We’ll manage risk and uncertainty to weave a safety net around you and yours. We’ll manage your anxiety, your sleep deprivation, your post-natal depression.
As your children hit their teenage years, we’ll manage their sporting injuries, their acne and their period problems, as well as sexually transmissible infections, mental health problems, migraine, asthma, and allergies. Day or night.
And you won’t need to ask for a referral letter, meet referral criteria or get insurance because we are the specialists that deal with all these problems. We’ll advise, educate, listen, and care. Sometimes we’ll prescribe, sometimes we will refer, but we’ll remain at the centre of your care.
We’ll steer you away from unnecessary, harmful, and expensive tests and medications while managing our precious stocks of antibiotics to protect our communities from antibiotic resistance.
As the spine running through our healthcare system, GPs are dynamic and flexible. We respond to public health crises. We have adapted to work through pandemics, bushfires, and floods.
When other facilities close, or become telehealth-only, we’ll still be there. We can still see you face-to-face, through our face masks and misted face shields. We’ll test you for COVID and, if you have it, we’ll work with other specialists to assess your risk and manage you accordingly. And we’ll treat all your other illnesses and needs during COVID. We’ll still listen to your chest, check your ears, palpate your abdomen.
And as your body begins to fray as you age, we’ll treat your hypertension, arthritis, diabetes, atrial fibrillation, high cholesterol, and kidney disease. We’ll bring in a team of allied health professionals around you. We’ll work with you to manage your conditions as if it’s a meeting of specialists. You, the expert in your own day to day illnesses, and we, who specialise in managing it.
Our early preventive work may well save you from strokes, heart attacks, diabetic complications, influenza, shingles, pneumonia and more. We’ll help screen you and your family for cervical, breast and bowel cancer. We’ll do your skin cancer checks and remove suspect moles, lumps, and bumps. We’ll help you lose weight, stop smoking and reduce your use of alcohol and other substances.
If life takes some tough turns, we’ll still see you, regardless of your income or insurance. We’ll still treat you with respect and dignity if you’re homeless, depressed, substance-dependent or live with schizophrenia. We’ll listen without judgement, counsel and help you make safer choices. We’ll prescribe and manage your clozapine, buprenorphine, methadone, antivirals for hepatitis or PREP for HIV.
And as you enter the autumn of your life, we’ll still care for you. When your hair is white, your eyes milky blue from cataracts and your skin translucent and peppered with the blemishes of age, we’ll listen to what care you want and what you don’t.
If other specialists say you’re now too frail or too confused or too complex to come to their clinic, we’ll still treat you. We’ll help you with your dementia and your falls and your incontinence. We’ll handle your comorbidities and multiple medications and spot drug interactions and side effects. We’ll plan your end-of-life care and, when that time comes, we’ll care for you at home, if that’s what you want.
And we will care. Not in a commodified or profit-driven way but because we know you, your values, your family, and there was always something we liked about you – because there is in all our patients – even though you dismissed what we do.
When it’s over, we’ll embrace your wife and children, and we’ll sit and listen as they press tissues to their eyes. And one day we may care for your grandchildren, too, remarking on how alike they are to you.
And as we get older, we’ll pass on our specialist skills and knowledge and attitudes onto medical students and registrars. We’ll teach them to be proud of being specialists in general practice. We’ll help them to practise justly, and to provide care to everyone regardless of age, ethnicity, sexuality, gender, education, or income.
And we’ll teach them they are not, and never will be, ‘just’ GPs.
Yours,
The mum in the park who’s very proud to be a GP
Dr Claire Denness
16th October 2020
First published in newsGP, republished with permission
Remembering Juniper
Trigger warning: grief and loss touches us all
Read MoreI remember
I can still see her you know, in my mind’s eye. She was a petite, attractive woman with fine features and an air of graceful resilience. She was one of those people who brought a smile to your face when you saw she was in the appointment book, because seeing her was always pleasant. Not that she came in often – she was fit, healthy and took very little medication, so perhaps a few times a year – for repeats, a flu shot and routine checkups.
It was 1998 and I had been a GP for 6 years in the small practice in Melbourne at which Eva was a long standing regular, along with her daughter-in-law and grandchildren. Her husband and son were also regulars of the practice, but usually consulted my male colleague. It was late winter 1998 and, unusually, Eva was accompanied by her husband Jani as she came into my consulting room.
After we settled into our seats and exchanged pleasantries, I opened with my usual line of “So, what brings you in to see me today?” and Eva proceeded to describe a recurrent, seasonal burning sensation in her toes which seemed to be worsening as the years went on. As I bent to examine her feet, I could sense a tense interaction between Eva and Jani. “Tell her,” Jani urged, “tell her how this started”. I looked up. Eva seemed annoyed, and shook her head very slightly. I sat up and looked between the two, curious at this undertone between them, unprepared for what was about to be revealed next.
“It started in the concentration camp” Eva stated, flatly, looking to her feet, and this revelation seemed to please Jani, who nodded in support of his wife.
My favourite subject in senior was Modern History and I had studied WWII in detail, but although the practice I was a part of had a number of eastern Europeans of Jewish descent, to my shame, it had never occurred to me that this might be an important part of Eva’s history.
Jani went on to tell how they had both survived interments in concentration camps late in WWII. Hungarian by birth, they had witnessed the worst of human behaviour and Jani was convinced that Eva’s condition (chilblains) was directly related to the starvation and brutally cold conditions she had endured in the camp.
I listened, fascinated. I calculated that they would have been 14-18 years old at the time and suppressed a horrid thought of how incredibly vulnerable they would have been.
At some point, the conversation shifted onto politics. An election had just been called and Jani was keen to discuss the rise of the One Nation party. As a native born, bred and trained Queenslander, I had not been as surprised as many of my friends by the outcome of the 1996 election, reasoning that One Nation were giving voice to a disaffected minority. In my humble opinion, I thought that the movement would fizzle out. That, given enough rope, they would hang themselves, and I shared this opinion with Jani and Eva.
“I was there, in Hungary, and this is how it starts”. I can still hear his slow, deliberate emphasis. This.Is.How.It.Starts. and in that moment, I realised that I was wrong. This was not a case of “give them enough rope” but rather “all it takes for evil to triumph is for good men (and women) to do nothing” and I had, like so many moderates, been silent/done nothing.
“If she gets elected, we will move to Israel. We will leave all we have behind and move to Israel. We may be poor, but we will not stave and we will be safe!” Jani stated with a fierce determination fueled by a history I had only read about, but which he and Eva had lived. I could only nod in recognition of their journey, I had no words.
Pauline Hanson lost the 1998 election, but come election night 2016, as I saw her triumphant face on the TV screen, I found myself transported back to that consultation room.
“Those who cannot remember the past are condemned to repeat it.” (George Santayana)
Jani died of a heart attack and I had lost track of Eva after moving in 2000.
I don’t know how to do this, but Jani and Eva, #Istandwithyou. There is no them and us, there is only us, one species, inhabiting one planet. Different tribes, cultures, language and religions, but only one species. Kindness and love must win, the lessons of history, both that written in the past and that unraveling as I type, surely teach us that bigotry and hatred are paths to destruction and grief.
Those things that unite us are greater than those things that divide us.
And I remember.
Dr Adele Victoria
July 15, 2016
Silent suffering
You know how drowning doesn't look like drowning?
It’s not all loud yells for help and splashing
It’s quiet
Because that person is using all their energy, using everything they have just to keep their head above water
Mental health is like that too
I think people expect that someone drowning in their mental health struggles should have obvious signs
But we don’t (always)
We are spending all our energy just keeping ourselves afloat
Getting out of bed, working, raising our families
There’s nothing left for splashing about and screaming out for the help we so desperately need
So we just keep going and going
Until we can’t anymore
And we silently sink
And everyone wants to know why there were no signs
Maybe there were
Just everyone was looking for the screaming and the splashing and missed the silent suffering
Dr Emma
2019
“Are you going to be a specialist? Or just a GP?”
As a medical student and junior doctor in my hospital training years, I was often asked this question by friends, senior doctors and well meaning patients. It really grated on me, that one little word: “just”.
I always thought I’d become a GP. As a teenager, I was inspired to study medicine by my own GP who had always looked after my family with such care and compassion. As I went through my training I dabbled with the idea of other specialties; I was fascinating by the life stories of my geriatric patients, I loved the cute-factor of paediatrics, I was hooked on the emotional highs and lows of obstetrics, I enjoyed the team atmosphere of the emergency department. But I think, deep down, that I always knew I liked ALL of medicine too much and that above all I wanted to make a meaningful difference to my patients’ lives.
For me, GP was the obvious choice.
Nowadays, when I tell people that I’m a GP, they ask instead “So are you going to specialise in anything?” They don’t seem to understand that I HAVE already specialised. I’ve specialised in General Practice (and GP obstetrics) by doing an additional 4 years of training on top of my medical degree and internship. I am officially registered with the Australian Medical Board as a “Specialist General Practitioner”.
This has been a conscious decision; I haven’t just become a GP by default.
So to be asked these sorts of questions always seems so unfair. It implies that “GP” and “specialist” are two diametrically opposed alternatives, and that GP is the lessor of the two. If you’re smart, ambitious, passionate and successful you become a specialist. If you can’t get into anything else or if you want the easy option, you become a GP. It’s seen as a back-up option, not as a worthwhile career in itself.
The specialist vs “just a GP” dichotomy also perpetuates the idea that GPs are not “experts” in their own right; that GPs are the amateur doctors that do the easy bits of all the other specialties and then refer on when it gets too complicated.
I’d like to dispel that myth. GPs ARE experts. We are the expert in each and every one of our patients.
We are also the experts in:
· Preventative medicine
· Undifferentiated illness
· Chronic disease management
· Complex multi-comorbidity
· Judicious use of finite medical resources
· Coordination of the health care team
We do these things better than anyone else. In fact, studies (see here and here) have repeatedly demonstrated that an increasing number of primary care doctors results in better health outcomes overall, a higher quality of health service and at a decreased cost. Whereas an increasing number of specialists is associated with higher costs and poorer quality of care, including higher overall mortality. So, as a group, GPs do a far better job at improving health outcomes and for less cost compared to specialists.
The reality is that General Practice is an enormously rewarding, challenging and varied career and that no two days are ever the same. We have no idea what is going to walk through our door next and it could be anything from an infant with a fever, a pregnant lady with pre-eclampsia, an elderly patient with new onset atrial fibrillation, a young man suffering with crippling anxiety, a parent grieving the death of a child to a full-blown heart attack. And all of these medical conditions come with added layers of complexity from the patient’s personality factors, social circumstances, family situation, expectations, medical co-morbidities, values and beliefs.
To my patients: I know you may never understand the intricacies of medical training, but I want you to know that out of all the career paths on offer, I chose to be your GP; to be the person that you turn to in your time of need, to see you as a whole person and not just a diseased organ, and to be the one who helps guide you to health and wellness. I hope you know that I feel truly privileged to be your doctor.
In answer to the original question, no I’m not “just” a GP.
I’m a broadly-skilled, sub-specialised, expert GP, providing a damn fine health service to my patients and my community.
And I absolutely love it.
Dr Penny Wilson
September 16, 2013
Republished, abridged, with permission. Full version available here
Finding Hope
Seven years. It took seven years for her to open up. Seven years to start to tell her story. Seven years of repeat medications. Seven years of small talk. Seven years of watching her twist as her back pain took hold. Seven years of hearing snippets about how insecure she felt in her job. Seven years.
And then came an event so devastating that there was no one else to tell. So devastating that it ripped the scab off her wounds and left her deeply, deeply pain-ridden, damaged inner self exposed and vulnerable. So devastating that the only logical response was to contemplate suicide.
Merciless devastation.
“Please stay.”
I don’t remember what else I said that day, but I do remember saying “Please stay”.
I remember because she remembers.
Traumatised, abused, misunderstood, labelled. Navigating the world through shrapnel. Nowhere is safe. Systems that failed. Carers who didn’t care. Helplines who didn’t help. Professionals who walked away, no risk of attachment issues because there was no one who stayed around long enough to attach to.
Months and months of slowly, cautiously discussing the abuse. The betrayals. Those who looked the other ways. Small, infrequent acts of kindness. Achievements not seen as such as the endless reel of negativity plays over and over and over and over in her head.
And yet. Writing. Powerful poetry, excellent essays
Desperately reaching forward, communicating, educating
Increasing my understanding, the understanding of others
Bridge building
Generous. Kind. Compassionate
Beaten, berated but not broken
A little light in the darkness. Journey not completed, but underway
A glimmer — did I really see it?
Did I imagine it?
No, there it is again!
A glimmer of hope
A sense of purpose
Hope, rising from the ashes
“Drench yourself in words unspoken
Live your life with arms wide open
Today is where your book begins
The rest is still unwritten“ Unwritten, Natasha Bedingfield
Dr Adele Victoria
January 14, 2020
The cancer journey
Too often, I hear the phrase that someone has "lost their battle" with cancer
This makes me angry - this is not a war with bayonets, bombs and bullets
Cancer does not
shatter hope
corrode faith
destroy peace
suppress memories
silence courage
invade the soul
kill friendships
or conquer the spirit
Cancer does not cripple love
These people precious to me have not "lost"
They have lived, endured, loved, been angry, cried but continued to live, until the very end.
Dr Gretchen Hitchins
December 18, 2017
With thanks and acknowledgement to those who work in palliative care and to others whose writing is similar
First published on the private Facebook group, GPs Down Under Dec 2017
It's quiet
Usually in summer we hear sirens, jet skis and illegal fireworks, brought on by the influx of Sydney tourists, but this summer I can only hear the relentless wash of the waves on Collingwood Beach.
It’s almost a relief, until I remember why.
Relentlessness is what characterizes this summer’s fire emergency.
It’s not a single event where the plane has crashed, the waters have risen, and you can be pretty comfortable that the recovery phase is what comes next.
A month ago during our regular treatment trips to Children’s Hospital Westmead, the ward was full of smoke.
On New Years Eve I was on a pontoon boat with my husband and daughter getting home to our other daughter, because the Princes Highway was closed at South Nowra.
This time last weekend I was setting up our little room at St George’s Basin Country Club evacuation centre.
On Thursday I was prepping in case it happened again.
Last night the southerly buster threatened to push more fires up to us.
So far in Jervis Bay?
Nothing
The embers were defended by the unsurpassable New South Wales Rural Fire Service at Sussex Inlet, Basin View and Tomerong.
Our trees are standing, our kangaroos with joeys happily grazing on my green front lawn, our roads are open.
But here’s the thing - we have fires to our North, South and West.
We have dense bush that hasn’t been burned since 2001.
We have 2 months left of the longest, scariest bushfire season we have ever experienced.
We watch, in a bizarre mix of survivor guilt and vicarious trauma, while our friends and colleagues around us burn and struggle.
And we wait, hoping we will get through unscathed.
Dr Kate Mandelson, GP
January 11, 2020 #AustralianBushfires
First published on the private Facebook page, GPs Down Under
Sitting in the darkness
As I lay in bed at 4 am this morning, reflecting on the difficult life journey of a colleague, the following thoughts came to me and I hope you don't mind me sharing them.
Perhaps the most profound thing any of us do, as fellow humans, is to sit in the darkness with another.
No magic wands
No silver bullets
Just to sit and to be
Some pains run so deep there are no words
For those of you in the darkness, please know that you are not alone.
For those of us privileged to sit awhile with another, never let us forget how important this can be. How simple things, like an appropriate touch, can make a difference.
Stay safe. Be kind to yourself and to others.
Merry Christmas
Follow up: Following on from this morning's musings and mindful of a reflection about (not) "feeling the need to switch on the light" I thought I'd share the following words. I have always been taken by the last two sentences, especially when "all" you seem to be doing is sitting in the darkness.
"Every bit of light, every small gesture is needed. It is not our task to judge the worthiness of our own light or even to know if it is seen. We are too quick to measure our lives by dramatic moments, too ready to minimize the light that we shine into the small darkness of everyday life. It is not given to us to know who is lost in the darkness that surrounds us. We can only know that against even the smallest lights, darkness cannot stand. A sailor lost at sea can be guided home by a single candle. A person lost in the wood can be led to safety by a flickering flame. It is not an issue of quality or intensity or purity. It is simply an issue of the presence of light."
-- Kent Nerburn –
Dr Wendy Burton
Christmas Day, 2016
Originally published on the private Facebook group, GPs Down Under
Dad's last lesson
‘Practice on me, use me as a guinea pig,’ Dad would joke, presenting himself on the sofa for my nervous first-year-medical-student fingers to palpate and percuss.
‘Did you learn anything?’ he’d ask, his eager questioning draped in a thin veil of anxiety.
’It all seems okay,’ I would murmur, wondering if I actually had the skills to find an abnormality if there was one.
Twenty-two years later, he said the same thing: ‘Learn from me.’
This time, however, his anxiety was not veiled, but exposed for all to see.
This time, my father was a shrunken figure, sinewy hands resting on a distended abdomen that would have been a medical student’s delight. Within it lurked a huge, aggressive liposarcoma.
Hugging his cardigan for warmth, he patted the skin stretched tightly across his abdomen.
‘They say it’s rare and there’s not much they can do. But maybe you can learn something from me. Maybe I will be useful for your patients, somehow.’
And afterwards, as I adjust, shakily, sewing tentative stitches into a life that is differently shaped, I wonder if my dad’s death can be the silver thread in this new landscape. If it can help to sharpen my clinical skills, slow down the time meted out by the consulting room clock, soften and embolden my touch.
Dad’s palliative care nurses saw every grimace, heard every rattle and, seamlessly, relieved it all.
We could not give Dad all of his last wishes – we never got to have that last cup of tea with him overlooking the ocean – but he did die peacefully at home, with his family around him and, for that, I will forever be indebted to his wonderful palliative care team.
On what turned out to be Dad’s final night with us, one of the palliative care nurses asked me about his life.
I held Dad’s hand, silhouetted by the almost-dark sky, as I told her about the Catholic boy from Belfast who sang Irish folk songs, and who left to join the RAF. About the young man who married a Protestant, moved to Cyprus, ran the gliding club. I told her of distinctions in Latin and fluency in French and German.
The letters from my Dad’s specialists had noted ‘interesting clinical signs’, including nicotine stains on his fingers and nail-clubbing, but, oh, what those fingers could do.
Since Dad died, my patients have also lost loved ones. Fathers, sons, partners, best mates, beloved pets. Old age, inherited neuromuscular conditions, catastrophic stomach or bowel bleeds, lung cancer, heart attacks. Some of them I knew and some I didn’t. I used to trot out the reliable platitudes, conscious that I needed to show the patient I was acknowledging their loss.
Now, it hurts a bit more keenly. Now I know that my patient wants their loved one to be remembered, wants their name to be used out loud, not side-stepped.
They don’t want platitudes, just as I didn’t and still don’t. Maybe they want space and silence, maybe they want to cry and gulp back big, ungraceful tears, raging against a world that carries on revolving, regardless.
I try harder to find the time for that silence. The space to ask them if they want to talk about it today or maybe tomorrow.
I am very lucky to work in an incredibly diverse, busy, inner-city community health clinic. The stories that my colleagues and I hear, daily, can be hard to hear, stories that show us the very best, and the very worst, of humankind.
When my patients heard my news they showed me, in their own way, their kindness and empathy too. Firstly notes, cards and gifts appeared, rippling in on the tide of each new day: flowers, Greek biscuits, brownies, a vegetable peeler (‘Cooking helped me get through my own Dad’s death’), a Chinese acer tree (‘This was my beloved mother’s favourite plant. She would have liked you’), a fridge magnet of a cat from Cyprus (‘I remembered your Dad had worked in Cyprus’).
And then, from a community in which so many members have been damaged, forever, by actions of their own parents, or other trusted adults, came the spoken words and the physical gestures of kindness.
The 184 cm, 135 kg, heavily-tattooed motorcyclist who was subjected to horrendous abuse by his own father, and then incarcerated, aged 16, for attempted murder who, with the lightest of touches on my shoulder, whispered, ‘I’m sorry for your loss, mate’.
And the ex-heroin user who never knew her own Dad, and has acquired psychiatric labels throughout her life ranging from ‘borderline personality disorder/complex trauma disorder’ to ‘paranoid schizophrenia’. The lady who, by her own admission, hates physical contact, but asked me if she could hug me when I returned to work.
Maybe I can be a better GP for having felt the raw grief of a parent dying, for realising that I am loved a little bit less in the world now, that part of my harbour wall has gone and so I am less sheltered from life’s storms.
Maybe I have really understood now the beauty of life, its transience and fragility, and the immense privilege that is afforded to us when we become doctors. A privilege that is easy to lose sight of, sometimes.
Maybe I really understand now that grief is an inevitable human experience, but, from my patients, I have seen and felt the capacity of the human heart to heal, repair and love once more.
Dr Claire Denness
23rd December 2019
First published in newsGP, republished, abridged, with permission
I’m emotionally exhausted
I need to debrief and I am only too aware that I am so so so much luckier than some of my colleagues and many of my patients
I work in the Southern Highlands of NSW, Australia. I was unable to get in on Saturday because of the fire (road closure and evacuation orders), worked an extra shift yesterday and back again today
I was fully booked days ago
100% of my patients are fire affected
80% cried
50% had no home or didn’t know if they had a home to go home to
20-30% were fit ins as they were having trouble breathing, had chest pain, were people I will always fit in (pregnant, kids, cancer diagnosis, palliative care or just on my “must fit in list”)
10-20% Rural Fire Service, Fire NSW or State Emergency Service seeking help for acute injuries sustained yesterday
I’m keeping my kids close tonight as they sleep and looking for my knitting and a glass of wine….
I feel so privileged being safe and home
Dr Bek Hoffman
January 6, 2020 #AustralianBushfires
First published on the private Facebook page, GPs Down Under
Photo: Sir Ivan Fire Feb 2017
Emergency response
It is January 2020 and Australia is on fire. The following is a story from a GP on the front line who seized the initiative to safety net her community.
My colleague Dr Lee Simes and I have put together a medical room at the St George’s Basin Country Club evacuation centre, and have a list of 5 local GPs and 8 local nurses who are ready to come in as needed. We decided to offer our services because we expected our community might be isolated by fires for days, possibly without power. The evacuation centre team welcomed us with open arms, and our conversations since then have been about “why don’t we have General Practice embedded within our emergency and evacuation plans?”
Calling an ambulance or driving to the hospital are absolutely the right thing to do for the right patient at the right time, but when there are embers and dense smoke closing our roads, maybe having patients seen by GPs and community pharmacists - with the right equipment, training and experience, working with NSW Health and St John Ambulance volunteers - ought to be an option included in the emergency plan, and not just something that the local on-call doc and pharmacist put together on their own. The experiences from our GP and pharmacist colleagues further south demonstrate the value and importance of the primary care team when the ambulance and hospital are simply not available.
I’m looking forward to meeting with the right people in leadership positions to make sure this can be done for when the next (inevitable) fire emergency comes around. For now, I’m just looking forward to packing up my gear, blissfully unused I hope, a few days from now .... fingers crossed!
Dr Kate Manderson
GP from Nowra on the NSW South Coast
January 4, 2020
The pocketknife clinic
It was the year 2000 and I was running the GP and worksite medical services for a construction site in Matola, Mozambique.
The site was very busy but I had been struck down by my third bout of malaria and I had to follow my own rules and stay away from work for five days until the medication had a chance to work.
Then disaster struck – a massive flood hit Mozambique and large parts of the country were inundated with water.
Slowly international aid started arriving, but it was patchy and there was great need. I could stay at home and feel sorry for myself while recuperating or I could make myself useful – I chose the latter and hitched a ride in the back of a transport chopper to one of the relief camps 300km to the North.
The camp was extremely basic – half of it had a foot of water over it and the Puma could not even land – we had to jump the last metre to the ground – it was rather unnerving to see the snake slither away just as I hit the water.
The refugees were housed in lean-tos made with tarpaulins and branches and they were desperate. Our only supplies were in a marque tent manned by a small group of volunteers who all looked like they had barely left school. My medical supplies consisted of my personal tools and a few boxes of supplies sent from charities abroad, mostly from Australia.
My first challenge was to find a place to work in. I had a tarpaulin, crepe bandages and my Swiss army knife. So that afternoon, I built a clinic.
The next morning I looked out and there was a line of people stretching over a 100m, waiting to be seen.
It turned out that there had been no medical services of any sort in that area for nearly 30 years.
In a country ravaged by nature and civil war they thought this one GP with his stethoscope and a few boxes of basic supplies could cure them of anything from heart failure to cancer.
I tried my best over the next three days, then I had to leave. I had a worksite with 10, 000 construction workers that depended on my expertise to keep them safe from malaria, cholera and work injuries.
Did I make a difference?
I would like to think so, but how do we ever know?
Dr Thinus van Rensburg
Too close for comfort
He wasn’t supposed to be wearing these shoes, you know.
These were his new shoes, bought for the start of the school year.
You don’t wear new shoes when mowing, you wear your old ones.
I didn’t realise the mowing had stopped, but I did hear the front door bell.
He was ashen faced when I opened the door. “What’s up?” I said and he silently pointed at his shoe.
At the hole in his shoe.
At the hole in his shoe through which his (perfectly intact) sock was showing.
We sat him down. Reassured him it was OK. Took the sock off and marveled that the nail was split but the sock was intact. Heard how, when mowing up the hill, the mower had slipped back and cut through the top of his new shoe.
And we were very glad he was wearing these shoes.
His new shoes.
The old ones were a much closer fit.
Best value-for-money pair of shoes.
Ever.
More careful mowing in future.
Dr Wendy Burton
January 3, 2020
Pennies for umbilical hernias only
After my parents died, I was cleaning out their medical equipment and I came upon this tin with "Pennies for umbilical hernias only" written in my mother's neat hand. Inside was, indeed, a collection of pennies.
My dad in particular was a man of science. A straight up and down widely-read, show me the evidence or else fellow with an incredible memory. Mum was more flexible in her approach but neither were out there on the fringe. Both were country GPs.
So, did they believe this worked?
Was this a placebo? So parents would feel something was being done while nature took its course?
I never asked, so I'll never know, but I keep this tin with its pennies in my consulting room.
It reminds me to hold knowledge lightly.
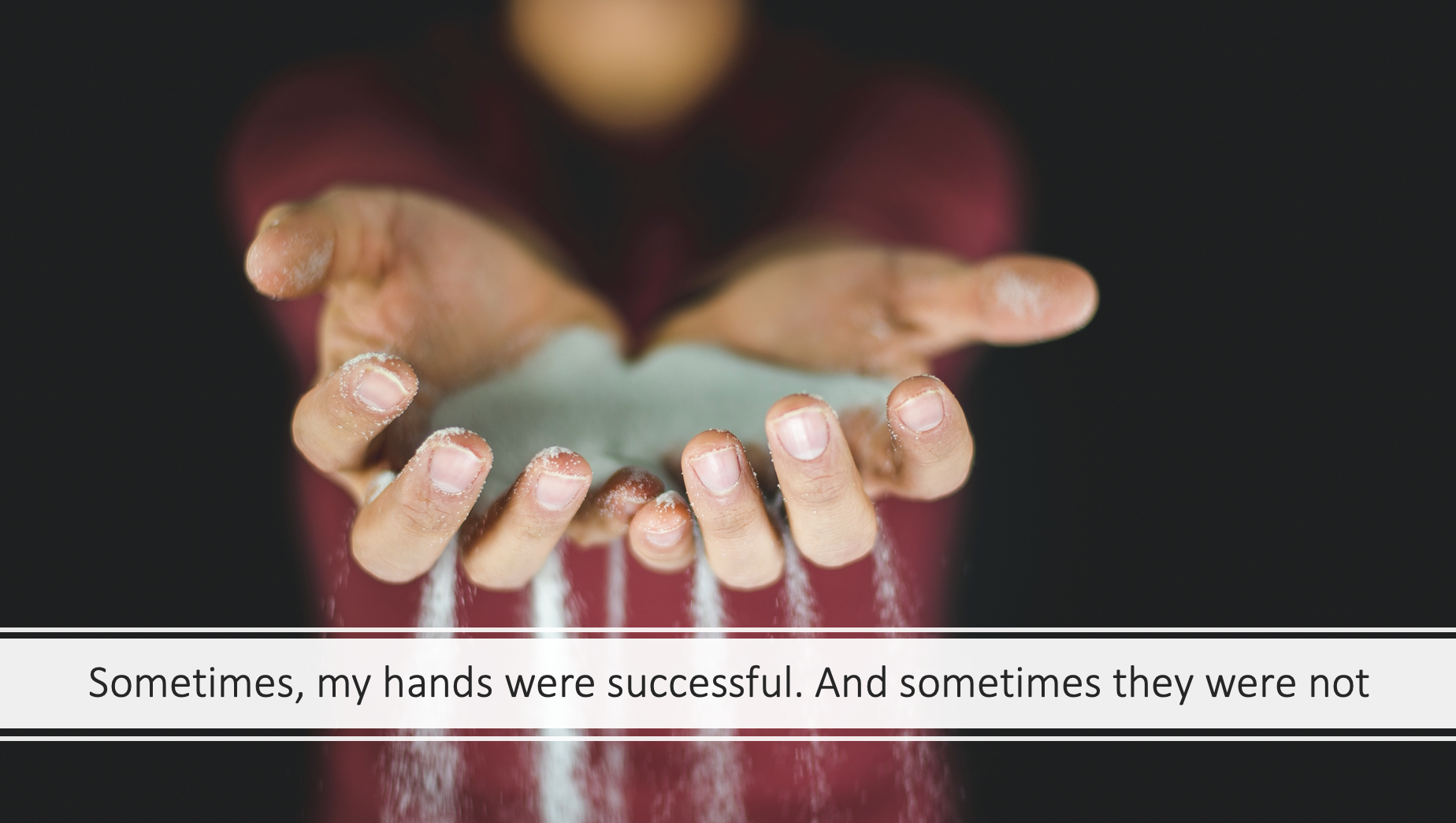
My hands
My hands have tried to save lives
I never really liked them when I was growing up. I felt they were always a bit too big, the veins too prominent. My nails were never shaped neatly but always slightly ragged and cut hastily, a bit too short. I look down at them today, despite my efforts to touch-type, and notice that, still, the nails are a bit too short; the skin dried out by hand washing and now also a bit wrinkly. But now I take less notice of their outward flaws, as I remember what they have done as the tools of my trade for the last 13 years.
My hands have brought life into the world. They have been the first hands to touch brand new, warm, slippery, vernix covered skin. The first hands to write new names on tiny wrist bands. To stretch yellow knitted hats over tiny heads.
My hands have tried to save lives. Shaken as they applied the pads or paddles and pressed ‘shock’. Tapped to find a vein. Tightened a tourniquet. Tapped again. Trembled as the cannula pierced flesh. Hoped. Interlocked and compressed. Felt the rhythmic bounce of the sternum underneath them.
They had to stop their compressions; instead fold together, poised, beneath a bowed head. Touch a colleague’s shoulder to signal that their hands should also stop. They have felt cold flesh under their fingertips and drawn up the hospital sheet to cover the indignities of resuscitation. They have written in black ink to confirm the finality of a life passed. And paused to wonder what those hands had done in that life, what hands had held that person dear.
My hands have communicated as they helped me listen to stories. Stories of all things human - joy, anger, fear, grief, trauma, addictions. My hands have passed tissues, rested on other hands, arms, shoulders. My hands have embraced, because, sometimes, that is all that can be done.
My hands have prevented influenza, pneumonia, shingles, HPV, measles, meningitis, hepatitis, and more. How many deltoids, old and young, have they exposed and how many vaccinations have they administered? Applied band-aids and stuck stickers on sweaters. Tousled brave heads and signed green books.
And how many times have my hands pulled the curtains around the examination couch, palpated abdomens, pelvic organs, found elusive cervixes? Swabbed and smeared. Inserted IUDs, ring pessaries, contraceptive implants. Prevented and detected cervical cancers; imparted contraceptive choice.
I think about how my hands have managed acute and chronic diseases. Checked blood pressures, oxygen saturations, peak flow readings, dipped urine samples. Felt for a pulse: regular, irregular, too fast, too slow, thready, bounding or quickly collapsing. Feeling again. Necks, wrists, feet, knees, groins. Auscultated and percussed lungs and abdomens. Pricked fingers and toes; swung tendon hammers. Squeezed skin nodules, held dermoscopes, ophthalmoscopes and otoscopes; checked temperatures of hot foreheads, swollen shins, sore knees.
My hands have helped me explain anatomy, diagnoses and treatment plans. They have drawn pictures: diverticulae, enlarged prostates, vertebrae, mostly it seems (from an unofficial audit). They have written and typed notes, referral letters, medical forms, Centrelink reports, radiology requests; checked interactions, issued prescriptions. They have written instructions. And re-written them, more clearly.
My hands have been the tools for teaching medical students and GP registrars their trade too; passing on skills and experience etched in mine to hands that are less wrinkled.
And my hands have made mistakes. They have written the wrong doses of drugs, missed an important clinical sign. My hands have held my head in dark, lonely on-call rooms, blown my nose, wiped away my tears-and those of colleagues.
These are my tools-my hands, the hands of a GP.
Dr Claire Denness
First published on the RACGP History page, under Tales from the Tools
My stethoscopes
My stethoscopes. I had several. They were special, awe inspiring tools and badges of my new life and identity. I inscribed them with my name and learned to care for them - by trial and error. My first stethoscope – a gift from my proud parents - was usually crammed into a pocket of the short white coat I wore around the wards. One day, the tubing split. I learned the most durable way to wear it was draped around my neck.
I slowly and progressively learned to use it - to keep it clean, to not transfer infection and how to wield it without mutual embarrassment to the patient’s benefit. I built up a library of sounds in my own head and developed a sense of what was normal, what was not normal but not pathological and what was definitely pathological.
What episodes stick in your mind?
I remember when it did not work. When I could not get a BP reading because the BP was too low for Korotkoff Sounds, because I was in the back of an ambulance going lights and sirens to hospital, when I was attending to a patient in dire peril and the pounding of blood in my ears blocked out any other sound.
I listened and no noise came from one side of the chest.
I took a slow deep breath and eventually learned to focus on the needs of the patient - my fear served no function except as a distraction.
I heard the wheeze of asthma, the rales and crepitations of infection and the pleural and pericardial rubs, the hollow echoes of cavitated TB. There were things absent that should have been present and vice versa. I heard the unilateral wheeze of a stone in the right bronchus, of a compressive cancer. Far too often, I heard nothing and having heard nothing I turned to the nearest table and completed the Death Certificate.
I remember the roadside trauma, the cricothyroidotomies I had to do. I recall the anaesthetics. Did I really do all that?
I remember all the techniques I was taught by those who had seen it all, done it all and were only too glad to have an eager pair of ears to finally tell. They had so many stories bound up in medical confidentiality that they could not share with family or intimates. Finally, as my teacher they could unload. Their passion imprinted their stories into my consciousness – I can see them still. May they rest in peace. In spite of my encouragement, they never wrote their life stories, which is probably why I have become a researcher, a teacher and now RACGP Victoria Historian - to see that they are remembered. They learned their craft by the trial and error of everyday practice. They had paid a high price for their knowledge - if I or any other doctor could be spared by their experience, they will rest happy. “Chris, experience is what is left when you survive your errors.”
Dr Chris Hogan
First published on the RACGP History page, under Tales from the Tools
Unk
Lionel Nicholls never married. He had grown up in Woolgoolga. He lived in a one room fibro shack next to his nephew Jack’s house, close by the beach. He had been a fisherman for much of his life, although he would have almost certainly have worked in the local timber industry intermittently, as well as on the Woolgoolga Jetty during times of peak demand. He was functionally illiterate.
His sole venture into the wider world was apparently his military service during the Second World War with the Australian Army. The story I remember best was his regular description of hair-raising trips through the mountains of Syria in a frigid winter, driving large trucks along perilous roads.
Unk’s fishing boat had been destroyed in the big cyclone of 1937. The same storm washed about 100 metres of Woolgoolga Jetty into the sea. Quite possibly he was still struggling to make a living when war broke out in 1939, so joining up would have been a logical enough step.
I don’t know whether the army managed to tame Unk, as he was affectionately known to all and sundry, but no one else seemed to have. He was singularly undomesticated. He kept cats and regularly seemed to have new litters of kittens. In later years it fell to his nephew to gather most of them up and despatch them in the traditional rural manner. There was no vet in town in those days. Unsurprisingly his home was rather chaotic, and yet exuded a homely character.
When I came to town in 1981, he had been a long term patient of my predecessor, receiving daily Fortral injections for reasons that I never clearly elicited. At first I wasn’t game to challenge that practice as a young solo GP trying to make his way in a small country town. However, as the months went by I became increasingly uncomfortable giving a daily opiate injection to an old man who still managed to live in his own home, however humble, on his own terms and had no need or wish to go to hospital.
It took a little while to summon the courage to substitute his Fortral with something more benign. I had already worked out for myself that there was no rational discussion to be had on the matter with my grumpy old patient. I tried some vitamins, reasoning to myself that they might even help him, B1 and B12 came to the fore. I didn’t alter the daily routine, he still presented to the surgery every morning around 8.00 am, waiting with the swelling numbers of patients for the doors to be opened at 8.30 am (In those early days I didn’t have appointments, it was “first in, best dressed”. Fairly soon I started afternoon appointments, but left the mornings as they had always been for the good folk of Woolgoolga.)
Six days a week, Unk would be on my front doorstep around 8.00 am (For the first six months in my own general practice we lived out the back. The arrival of child number two and the desire for some sort of respite on weekends saw us find offsite accommodation in the latter part of 1981.)
Sundays were different, I went to him. I would take whichever of our children were capable of walking to give their mother a break. They were shy at first, but quickly learnt that someone had suggested to him that little children liked lollies. He took delight in handing over small bags to them, whilst the cats hopped on and off the bed, or exited via the window. I could see that it became one of the highlights of his week, so carried on as before. Interestingly, he never seemed to notice any difference when I injected him with thiamine occasionally, mostly normal saline, so I was at least able to avoid opiates. He was clearly dependent on the injection process, rather than the contents thereof. I think he was a lonely old man, quite reclusive, incapable of normal social interaction, and in need of some reason to have regular human contact. This we were able to provide for several years until the inevitable happened. He stroked out, and fortunately did not survive his trip to hospital, exiting this world having lived it generally on his terms. For me it was an important early lesson into the many and varied ways of humanity.
Of course, it would be impossible to practice in this fashion nowadays – such things would not be sanctioned in the current millennium.
Assoc Professor John Kramer
First published on the RACGP History page, under Tales from the Tools