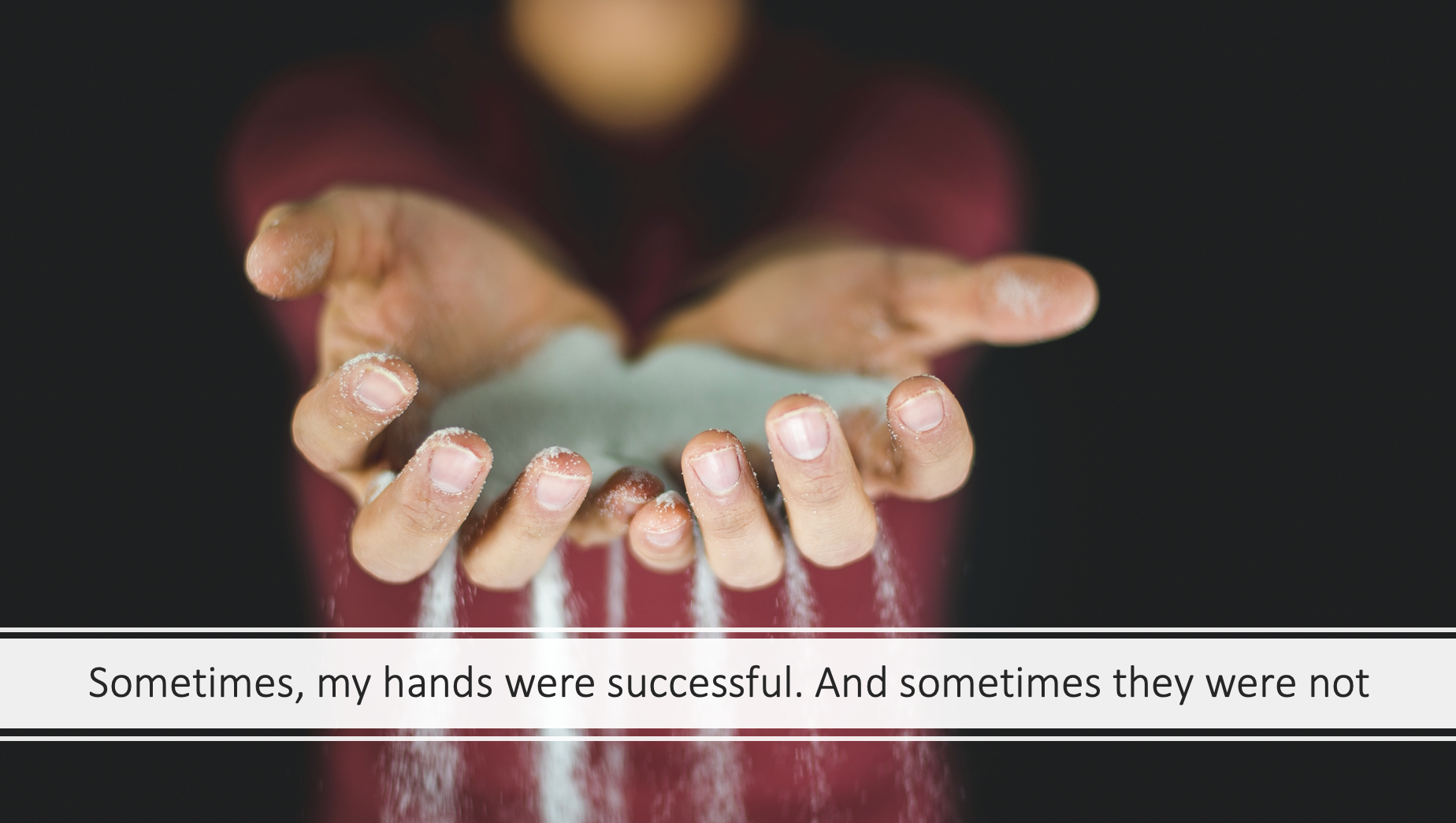
My hands have tried to save lives
I never really liked them when I was growing up. I felt they were always a bit too big, the veins too prominent. My nails were never shaped neatly but always slightly ragged and cut hastily, a bit too short. I look down at them today, despite my efforts to touch-type, and notice that, still, the nails are a bit too short; the skin dried out by hand washing and now also a bit wrinkly. But now I take less notice of their outward flaws, as I remember what they have done as the tools of my trade for the last 13 years.
My hands have brought life into the world. They have been the first hands to touch brand new, warm, slippery, vernix covered skin. The first hands to write new names on tiny wrist bands. To stretch yellow knitted hats over tiny heads.
My hands have tried to save lives. Shaken as they applied the pads or paddles and pressed ‘shock’. Tapped to find a vein. Tightened a tourniquet. Tapped again. Trembled as the cannula pierced flesh. Hoped. Interlocked and compressed. Felt the rhythmic bounce of the sternum underneath them.
They had to stop their compressions; instead fold together, poised, beneath a bowed head. Touch a colleague’s shoulder to signal that their hands should also stop. They have felt cold flesh under their fingertips and drawn up the hospital sheet to cover the indignities of resuscitation. They have written in black ink to confirm the finality of a life passed. And paused to wonder what those hands had done in that life, what hands had held that person dear.
My hands have communicated as they helped me listen to stories. Stories of all things human - joy, anger, fear, grief, trauma, addictions. My hands have passed tissues, rested on other hands, arms, shoulders. My hands have embraced, because, sometimes, that is all that can be done.
My hands have prevented influenza, pneumonia, shingles, HPV, measles, meningitis, hepatitis, and more. How many deltoids, old and young, have they exposed and how many vaccinations have they administered? Applied band-aids and stuck stickers on sweaters. Tousled brave heads and signed green books.
And how many times have my hands pulled the curtains around the examination couch, palpated abdomens, pelvic organs, found elusive cervixes? Swabbed and smeared. Inserted IUDs, ring pessaries, contraceptive implants. Prevented and detected cervical cancers; imparted contraceptive choice.
I think about how my hands have managed acute and chronic diseases. Checked blood pressures, oxygen saturations, peak flow readings, dipped urine samples. Felt for a pulse: regular, irregular, too fast, too slow, thready, bounding or quickly collapsing. Feeling again. Necks, wrists, feet, knees, groins. Auscultated and percussed lungs and abdomens. Pricked fingers and toes; swung tendon hammers. Squeezed skin nodules, held dermoscopes, ophthalmoscopes and otoscopes; checked temperatures of hot foreheads, swollen shins, sore knees.
My hands have helped me explain anatomy, diagnoses and treatment plans. They have drawn pictures: diverticulae, enlarged prostates, vertebrae, mostly it seems (from an unofficial audit). They have written and typed notes, referral letters, medical forms, Centrelink reports, radiology requests; checked interactions, issued prescriptions. They have written instructions. And re-written them, more clearly.
My hands have been the tools for teaching medical students and GP registrars their trade too; passing on skills and experience etched in mine to hands that are less wrinkled.
And my hands have made mistakes. They have written the wrong doses of drugs, missed an important clinical sign. My hands have held my head in dark, lonely on-call rooms, blown my nose, wiped away my tears-and those of colleagues.
These are my tools-my hands, the hands of a GP.
Dr Claire Denness
First published on the RACGP History page, under Tales from the Tools